Pandemics make for great drama. No TV or movie season is complete without at least one viral apocalypse—preferably involving zombies—sweeping the globe. But pandemics aren’t just science fiction. They have happened—and perhaps will happen again. (For more, see “Breakthrough: Fighting Pandemics” November 1 at 9 p.m. (ET) on the National Geographic Channel.)
Pandemics make for great drama. No TV or movie season is complete without at least one viral apocalypse—preferably involving zombies—sweeping the globe. But pandemics aren’t just science fiction. They have happened—and perhaps will happen again. (For more, see “Breakthrough: Fighting Pandemics” November 1 at 9 p.m. (ET) on the National Geographic Channel.)
So, quick quiz: what’s the best way to motivate people to plan for the next pandemic?
- Be honest about the real risks, explain how these risks can be managed, demonstrate what is already being done and how successful it has been, and ask the public to support the necessary investment to maintain and extend that effort.
- Whip the public into a frenzy with scientifically implausible doomsday scenarios and imply that nothing is being done to prevent them.
I guess you know where I’m going to come down on this.
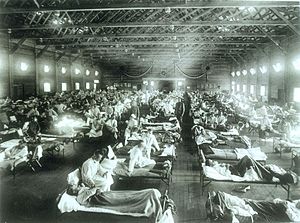 I take pandemics seriously; I spent nearly a decade studying the influenza virus that caused the granddaddy of all pandemics in 1918 and 1919. Estimates put the death toll between 20 and 50 million. The only other true pandemic—an outbreak of infectious disease that spreads rapidly across multiple continents or around the world—of the last century is still with us: HIV/AIDS has killed 39 million people since 1981, and nearly 37 million are living with the virus now, with just over one million people still dying every year.
I take pandemics seriously; I spent nearly a decade studying the influenza virus that caused the granddaddy of all pandemics in 1918 and 1919. Estimates put the death toll between 20 and 50 million. The only other true pandemic—an outbreak of infectious disease that spreads rapidly across multiple continents or around the world—of the last century is still with us: HIV/AIDS has killed 39 million people since 1981, and nearly 37 million are living with the virus now, with just over one million people still dying every year.
There have been other serious outbreaks of infectious disease: terrible as it was, the 2014 Ebola outbreak was confined to West Africa and contained in a matter of months. It killed fewer than 10,000 people. SARS spread around the world but was rapidly contained, infecting fewer than 10,000 people and killing fewer than 1,000. Other emerging diseases—West Nile Virus, Middle East Respiratory Syndrome (MERS), avian influenza—have not spread in humans widely or rapidly enough to rise to the level of pandemics.
 But is the risk of pandemics growing? Many aspects of the modern world raise concern. We know that live animal markets, increased reliance on “bush meat” for food, and the massive displacement that climate change will cause, will all provide opportunities for infectious organisms to move into new territories, and “jump” species boundaries. And of course air travel makes it possible for infectious diseases that once had to sustain outbreaks for weeks to make it from continent to continent can now do so in hours.
But is the risk of pandemics growing? Many aspects of the modern world raise concern. We know that live animal markets, increased reliance on “bush meat” for food, and the massive displacement that climate change will cause, will all provide opportunities for infectious organisms to move into new territories, and “jump” species boundaries. And of course air travel makes it possible for infectious diseases that once had to sustain outbreaks for weeks to make it from continent to continent can now do so in hours.
On the other hand, advances in medicine, diagnostics, surveillance and communications put us in an ever stronger position to detect, contain, and treat emerging infectious diseases. In 1918, some 90% of deaths were caused by bacterial infections of lungs weakened by the virus. These deaths would now be preventable by antibiotics. (Nota bene, stopping the misuse of antibiotics and developing new ones needs to be right up there with pandemic prevention on the public health “to do” list.) It took 14 long years from the emergence of HIV/AIDS in 1982 to the development of the combination retroviral therapy that turned an invariably fatal disease into a chronic one. By contrast, SARS was first detected in November 2002, the coronavirus responsible was identified in March of 2003 and fully sequenced by April. The outbreak was contained by July.
So the legitimate concerns are balanced by some considerable assets. And besides, let’s not forget that viruses are not lurking behind every bush, just chomping at the bit to get into humans and wreak havoc around the world. As I wrote in two recent posts (“Viruses Are Not Omnipotent,” Parts I and II), viruses don’t jump between species willy-nilly. Viruses and hosts have evolved together for billions of years with the result that humans, along with every other cell-based life form, have elaborate and sophisticated immune systems to fend off viruses. Even though viruses tend to have high mutation rates (that’s one of their evolutionarily-determined adaptations), it is not trivial to accumulate the multiple mutations that are usually necessary to thrive in a new host.
Finally, lots of people are paying attention to the risk of a pandemic. Around the world, thousands of virologists, ecologists, epidemiologists, public health, aid, and disaster relief workers are collaborating to assess risk and plan for the worst. We know what we need to do: invest in basic virology and epidemiology research, build up health care capacity around the world, establish and maintain a comprehensive surveillance, diagnostics, and detection system, and make sure that public health authorities and emergency relief agencies around the world communicate with and trust each other, so that they’re ready to share information and coordinate their activities quickly and effectively. Not very sexy, perhaps, but certainly more effective than hysteria.
So let’s all take a deep breath and put the risk of a devastating pandemic in perspective. Panic may grab people’s attention for a little while, but it’s not a sustainable basis of support for sensible policy. Hysteria leads to poor policy. Hysteria leads to uninfected health care workers being placed under house arrest. Hysteria leads to holding on runways airplanes that have been nowhere near the outbreak area to check on passengers with fevers. Hysteria leads to closing schools in Ohio and Texas for no good reason. Portraying the natural world as a seething hotbed of viruses poised to invade humanity, and implying that we are helpless in their path, is not just plain wrong—it’s dangerously wrong.
Zombie photo credit: By Bob Jagendorf via Wikimedia Commons
Live animal market photo credit: "Chicken market in Xining, Qinghai province, China" by M M (Padmanaba01) via Commons